There is an alarming number of youths in psychiatric or behavioral health crisis stuck boarding in emergency departments, medical units, county buildings, jails, and even hospital parking garages. These situations are intense, and the needed interventions and services are scarce. The average time spent boarding is increasing, in some cases up to weeks or even months. This is a result of an underfunded and understaffed mental health care system, that is ever-changing.
Complex mental health needs:
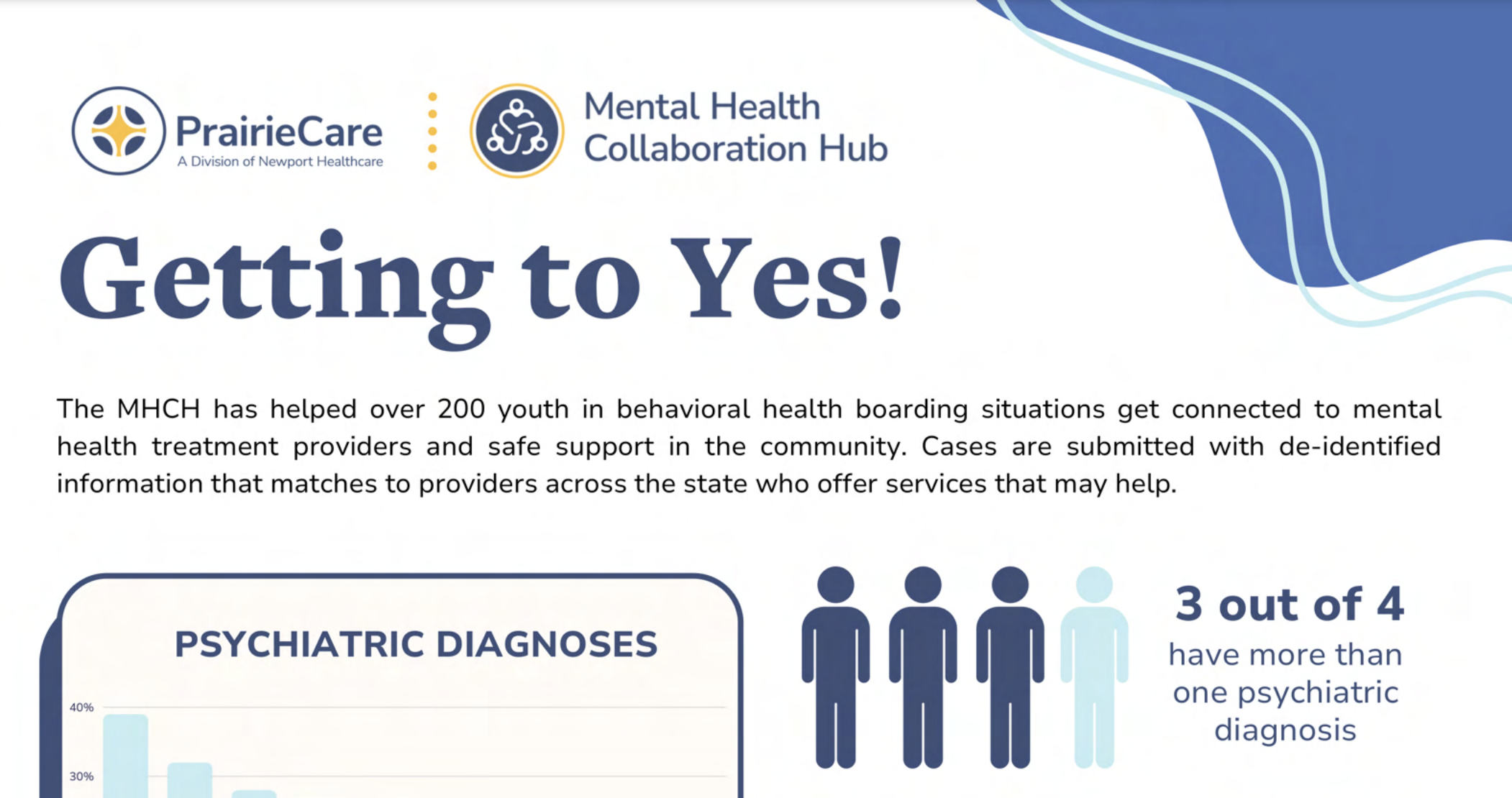
Most youth in boarding situations require complex mental health treatment provided by specific programs that range from group homes, children’s residential facilities (CRF), therapeutic foster care psychiatric hospitals, or psychiatric residential treatment facilities (PRTF). The American Psychiatric Association has defined nearly 10 different types of inpatient psychiatric beds. While not necessarily standardized, they range from state operated and community-based to specialized geriatric and forensic. For individuals with a mental or behavioral disorder, it is critical to have a clear diagnosis to understand the best treatment or intervention. The Diagnostic and Statistical manual of Mental Diseases (DSM) details more than 300 distinct conditions. The most common disorders in boarding cases are neurodevelopmental and externalizing disorders characterized by aggression, opposition, and maladaptive behaviors. Nearly 75% of these cases have multiple diagnosis that often include autism, developmental delays, ADHD, conduct disorder, and substance abuse. This requires the boarding settings to manage risk factors such as self-harm, elopements, suicidality, and combativeness.
A shortage of facilities:
More than 80% of counties in Minnesota have a shortage of mental health professionals. We have seen a 30% reduction of children’s residential treatment beds since 2020, and there are fewer than 200 operational inpatient psychiatric beds for youth in the state today. This is a startling lack of options that is further exacerbated by staffing shortages that limit these capacities. Minnesota currently has 93 licensed children’s residential facilities with a total of 1,586 beds, each serving a unique population. Facility sizes range from a handful of beds to large campuses with upward of 100 beds. Each facility serves a distinct age range, specializes in treating certain conditions, and may have acceptance criteria regarding gender, IQ, and county of residence. Additionally, certain certifications are required to treat conditions such as substance use disorders. Some specialties include eating disorders, autism, sexual misconduct, and obsessive-compulsive disorder. It is not uncommon for organizations to change acceptance criteria as they evolve, particularly the age range that they treat. These various specialties can be highly effective for some individuals, but the imbalance of capacity within each of them and the constantly changing landscape creates frustration for providers making referrals. Creating a shared understanding of the nuances in the different types of beds will strengthen our ability to collaborate and help kids.
Download PDF